
Katy Keenan holds a diffusion phantom made by colleague Michael Boss.
Magnetic resonance imaging (MRI) has become an indispensable tool for diagnosing, treating, and understanding a host of medical conditions, and the technology is evolving rapidly.
Until recently, however, many uses of the technology were hampered by a critical, but unanswered, question: How comparable are images taken on multiple different MRI machines, as is frequently the case in multi-site clinical trials, or on the same machine but months apart? The solution is a standard reference object (a phantom, or surrogate for different body sections or tissue types) that can be imaged at regular intervals to allow comparisons across MRI machines and across time points.
Thanks in large measure to standard phantoms developed over the past few years by Stephen Russek and colleagues in PML's Biomagnetic Imaging Standards project, those concerns are diminishing, and "quantitative MRI" – with rigorous metrics and identified sources of error – is becoming recognized as vitally important.
"Most of the basic measurement issues have been resolved," Russek says, "such as tumor volume as a function of time, better resolution, spatial distortion, and relaxation times. To speed progress, we recently acquired a 7 tesla* scanner. It has a small bore, but it's enough to characterize all the components of our phantoms that we fabricate for clinical use. We can now measure all their properties much more precisely."
But that doesn't mean that things are slowing down. "In fact, the need for standards is actually increasing," Russek says, "as researchers devise new procedures and imaging goals. So now we're finishing up the system phantoms and moving toward more specific applications.
"One is a phantom optimized for imaging diffusion, the way water moves in the body. But one of the key problems is that diffusion is inherently influenced by thermal effects. So we found that we needed to come up with an MRI 'thermometer.' Temperature is a big factor when you go from scanner to scanner. You can't just tell everybody to turn their thermostats down."
Other new research areas for the PML team include development of a prototype standard breast phantom, methods to help MRI manufacturers test the accuracy of their software algorithms, and research into low-field MRI – which uses magnetic fields as weak as the Earth's – for better contrast in imaging specific kinds of tissues and processes.
"It can be cheaper because you don't have to have a big superconducting magnet," Russek says, "but it also offers better tissue contrast in some cases, such as prostate cancer. It turns out the relaxation rates for certain tissue types tend to become larger at low field. It still hasn't been fully validated, so some of our work is to help validate those measurements."
Going with the Flow
MRI is conventionally associated with still images. But there are ways to configure the equipment so that it tracks changes in adjacent voxels (the three-dimensional counterpart of pixels) over time to show the motion of fluids. That is highly desirable for both medicine and anatomical studies.
"That's one of several types of MRI modalities that are not being fully utilized, in part because there are no standards," says Ron Goldfarb, leader of the Magnetics Group in PML's Electromagnetics Division. "So one of the next big things is a different type of phantom designed to measure perfusion, diffusion, and flow.
"For example, there are nerve tracks in the corpus callosum that connect the right and left cerebral hemispheres. As it turns out, water flows along those tracks, and you can image it with MRI. So you can get these beautiful colored streaks showing the nerve passages. But how do you calibrate that?"
Russek and company are finding out, with a concomitant emphasis on thermometry.
"It's very important for perfusion and diffusion studies, but also for certain kinds of procedures, such as RF ablation of tumors and heart and brain tissue, or in focused ultrasound heating where MRI both guides the focus and images the local temperature. The damage threshold, for short-term exposure, is near 50 °C. But there can be wide spatial variation in temperature linked to diffusion and perfusion. For example, a tumor with higher water content will have better thermal conductivity. So you need to know both the local flow and the temperature accurately.
"That capability doesn't really exist at present. There is a clear need for quantitative data on in vivo temperature. So in addition to our work on diffusion phantoms, project member Michael Boss is developing a local thermometer that uses a rare-earth chelate as a reference. It has a paramagnetic spin that is sensed by all the protons around it, and that spin effect is very temperature-dependent. It's very sensitive because a small change in temperature causes a big change in the resonant frequencies of the neighboring protons."
Trials and Horizons
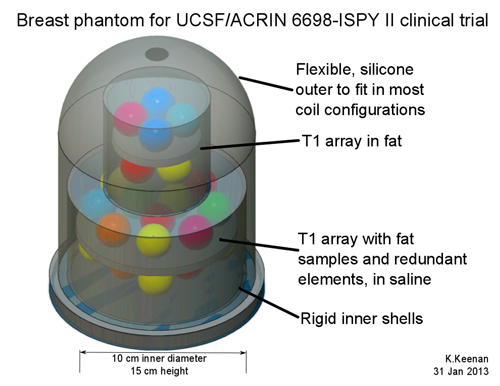
Another of the team's major initiatives is development of a standard breast phantom. Americans spend an estimated $16 billion every year on breast cancer treatment, and "several clinical trials are underway to assess treatment protocols," says team member Katy Keenan. "Quantitative MRI techniques are increasingly used as outcome measures."
In October 2012, NIST partnered with Dr. Nola Hylton to develop a breast phantom for the ISPY-2 TRIAL in collaboration with the American College of Radiology Imaging Network (ACRIN) and the Quantitative Imaging Network of the National Cancer Institute.
ISPY-2 is a multi-center clinical trial testing new breast cancer therapies and is being conducted at more than 20 sites nationwide. The goal of this trial is to validate MRI measurements, rather than invasive biopsy, as a response to treatment. It is essential that data be comparable across all sites. That calls for a phantom.
"Breast MRI is challenging due to the inhomogeneous mix of fat and fibroglandular tissues, which lead to image artifacts, as well as the range of breast sizes," Keenan says. "There are three broad goals for this breast phantom. First, to include fat and fibroglandular components specific to the MRI techniques of the ACRIN trial: tumor volume, proton-spin T1 relaxation time, and diffusion. Second, to include SI-traceable components similar to those used in the NIST system phantom. And finally, to ensure compatibility with all breast MRI coils on the market.
"Currently, we are finalizing the prototype design, and we will complete initial imaging of the breast phantom by the end of the summer. Industry and other clinical trials groups have already expressed interest in the breast phantom. We need to scale up production of the breast phantom to meet the needs of the community."
As research and phantom development proceed, "we're bringing standards to an area that has operated without standards," says Goldfarb. "But it needs and wants them."
* The tesla (T) is the SI unit of magnetic flux density. Ordinary clinical MRI systems operate at 1.5 T or 3 T. The Earth's magnetic flux density is about 50 microtesla.
When a patient is in an MRI device, the powerful surrounding magnetic field causes a large population of protons in the hydrogen atoms of the body's water molecules to align themselves to the field. A radio-frequency pulse is injected which "flips" the magnetic orientation of the protons, and is then turned off. The MRI equipment detects the times (T1 and T2) that it takes different properties of the protons to realign themselves with the applied field.
Those "relaxation" times differ according to the type of tissue the protons are in, as well as other factors. The differences are converted by software into a grayscale image.

