NIST Develops New Nondestructive Method for Assessing Bioengineered Artificial Tissues
Real-time technique noninvasively counts the number of live cells in a 3D artificial scaffold.
Engineering organs to replace damaged hearts or kidneys in the human body may seem like something out of a sci-fi movie, but the building blocks for this technology are already in place. In the burgeoning field of tissue engineering, live cells grow in artificial scaffolds to form biological tissue. But to evaluate how successfully the cells develop into tissue, researchers need a reliable method to monitor the cells as they move and multiply.
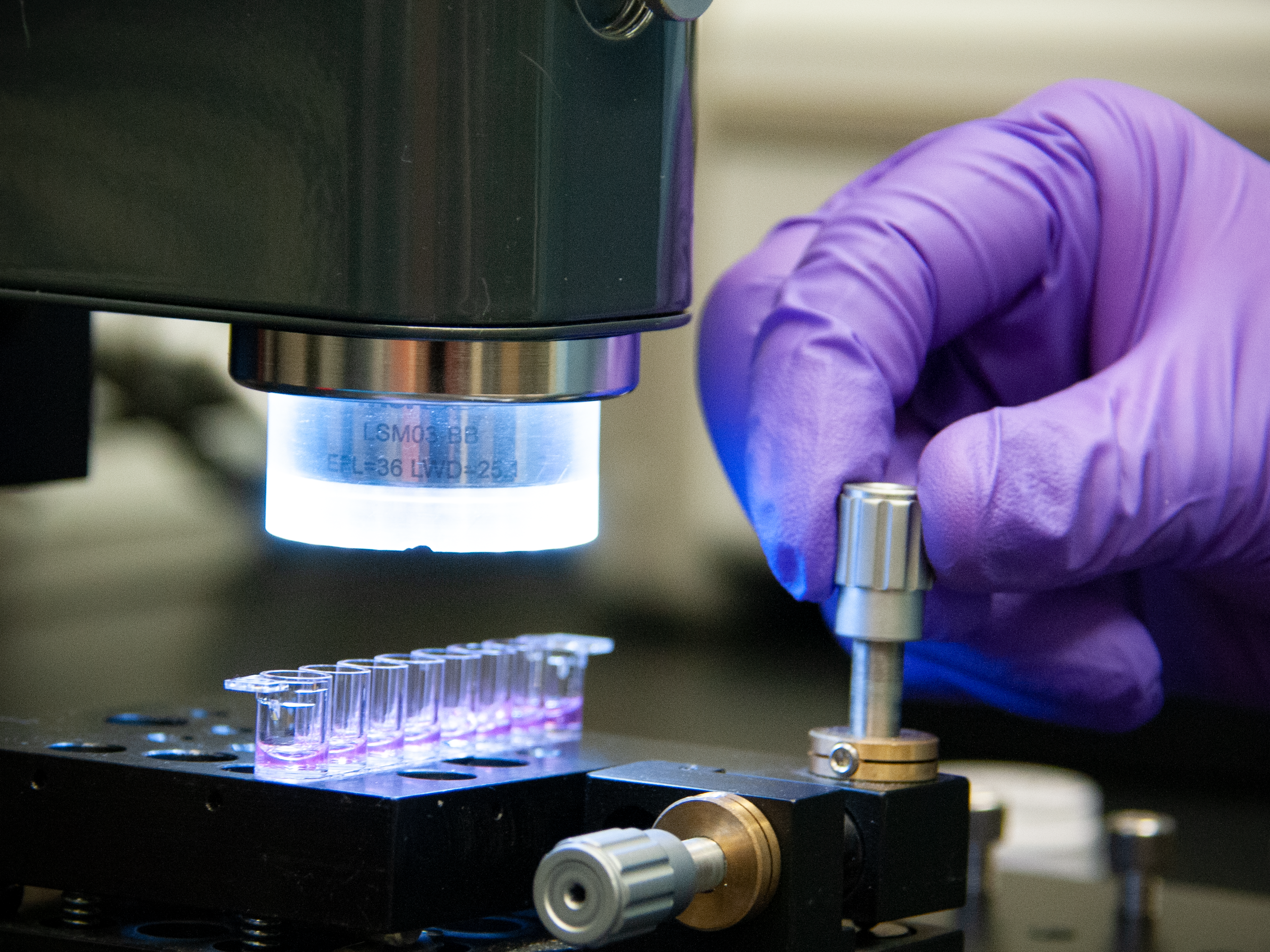
Now, scientists at the National Institute of Standards and Technology (NIST), the U.S Food and Drug Administration (FDA) and the National Institutes of Health (NIH) have developed a noninvasive method to count the live cells in a three-dimensional (3D) scaffold. The real-time technique images millimeter-scale regions to assess the viability of the cells and how the cells are distributed within the scaffold — an important capability for researchers who manufacture complex biological tissues from simple materials such as living cells.
Their findings have been published in the Journal of Biomedical Materials Research Part A.
First, researchers created a 3D scaffold system made from a network of polymer molecules that can hold large amounts of water, forming a type of material known as a hydrogel. The 3D hydrogel was then embedded with a type of human white blood cell that can reproduce endlessly.
Cells can be very sensitive to the environment in which they’re grown: If a researcher wants to study the growth of bone cells instead of breast tissue, they need to be cultured in different conditions. Moreover, the scaffolds that house the cells are also made from different materials and can serve a variety of purposes.
“The scaffold holds things in place, and it provides a micro-environment for whatever you want from cells. You could tune the scaffold to direct cells to behave in a certain way,” said NIST biologist Carl Simon.
The team then used a noninvasive imaging technique called optical coherence tomography (OCT), which is like an ultrasound test, except instead of sound waves it uses light waves.

“To determine if a cell is alive, we analyzed the optical signal created due to the motion of the organelles inside the cells,” said NIST physicist Greta Babakhanova, first author of the paper. The researchers detected organelle motion by shining light through the cells. They classified cells as live or viable when the organelles were moving, indicated by changes in the transmitted light.
The NIST method is noninvasive, and there’s no cutting or staining of samples. The method is also label-free: Cells did not need fluorescent molecules known as “labels” to be attached to them in order to be seen. Earlier methods required constant contact with the samples, which can be destructive and costly and affect the results. The new technique also reduces the time researchers spend on their measurements from hours to minutes.
The method also differs from earlier methods that rely on flat, two-dimensional samples. “The drawback of the existing techniques is that you can measure a certain number of cells, but you don’t know where they’re located. With this method we can image a one-millimeter cube of hydrogel and see where the cells are located within the gel,” said Babakhanova.
2D approaches also don’t work quite as well because they don’t closely mimic the 3D microenvironment that cells experience in the body, said Babakhanova.
As a next step, researchers are looking at applying the technique to study other properties, such as the structure of biofabricated tissue. “The OCT methods may be able to nondestructively measure specific structures that evolve as the tissues mature in real time as a measure of their readiness for implantation,” said Simon.
In the meantime, the method already meets an unmet need in tissue engineering, with its ability to monitor the number and arrangement of cells in an artificial scaffold without having to disassemble and destroy it.
Paper: G. Babakhanova, A. Agrawal, D. Arora, A. Horenberg, J. B. Budhathoki, J. P. Dunkers, J. Chalfoun, P. Bajcsy and C. G. Simon. Three-dimensional, label-free cell viability measurements in tissue engineering scaffolds using optical coherence tomography. Journal of Biomedical Materials Research Part A. Published online March 14, 2023. DOI: 10.1002/jbm.a.37528.

